Eczema Genetics, the Filaggrin Gene, and Environmental Influences
The epidermal barrier—our skin—is the body's first line of defense against the effects of the wider world, keeping those watery components of self safely contained within pliable, permeable, self-healing bounds, while keeping offending allergens, toxins and pathogens out. The structural protein filaggrin (or, filament-aggregating protein) plays a key role in forming this protective barrier. Any disruption in the expression of this protein is likely to influence the effectiveness of our body's first line of defense.
The discovery that mutations in the FLG gene that encodes for profilaggrin, a precursor of filaggrin, lead to epidermal barrier dysfunction is a significant breakthrough in understanding the genetic basis and pathogenesis of atopic disease, including eczema, allergies, and asthma. Loss-of-function mutations that prevent the expression of filaggrin in the skin have been shown to be a major risk factor for atopic eczema and eczema-associated asthma.
Eczema has long been recognized as a complex condition where genetic factors mix with environmental stimuli producing the disease in as many as 15% to 20% of children in developed nations, persisting into the adult lives of many of these children. In this article we'll take a look at the implications of the loss of filaggrin function and what it means for eczema sufferers.
"The discovery that null mutations in the filaggrin gene (FLG) are associated with atopic eczema represents the single most significant breakthrough in understanding the genetic basis of this complex disorder." —Filaggrin researchers Sara J Brown & Alan Irvine, 2008
Filaggrin and the Stratum Granulosum
When the genetic code of the FLG gene is transcribed in healthy individuals, the initial protein product expressed is profilaggrin, the main constituent of keratohyalin granules. These irregular-shaped granules are found in the stratum granulosum and exist in concert with tonofibrils, filamentous structural proteins that create a dynamic cytoskeleton in keratinocytes (basal cell) cytoplasm, as well as many other epithelial cells.
Profilaggrin is a poly-protein consisting of tandem repeats of the filaggrin peptide. When cleaved by proteolytic enzymes, profilaggrin yields multiple copies of the filaggrin protein that bind to and aggregate tonofibrils. Filaggrin is but one factor that apparently influences the dynamics of tonofibrils and similar cytoplasmic filaments.
As keratinization takes place within the keratinocyte, filaggrin-aggregated tonofibrils collapse the cytoskeleton, forming flattened squamous cells. Keratinization also destroys the cell nuclei in a mediated (timely) cell death. Further heavy cross-linking of this protein and lipid package (the bipolar lipids formed in keratinocytes while in the stratum spinosum) by transglutaminases complete the watertight, protective epidermal barrier.
These "dead" cells migrate into the upper layers of the epidermis, where they are sloughed off in the normal course of one's day, while being continually replaced with the squamous cells migrating from below. Deficient or missing filaggrin proteins compromise the epidermal barrier, making the barrier less able to provide a comprehensive defense against outside insults.
Filaggrin, and other barrier proteins, are known to be integral to the epidermal barrier. How dysfunction of these proteins compromises the barrier, in relation to the chronic inflammation and autoimmune mechanisms typical of atopic eczema or eczema-induced asthma, is still in need of further research and clarification. Yet even while much remains unknown, research is beginning to unveil the complexity of these mechanisms and their implications.
Skin Structure
Our skin is a dynamic system, constantly shedding its outermost layers as it replaces those lost epidermal cells with new cells, all the while maintaining a flexible, protective barrier that keeps water in and pathogens out, regulates body temperature, and mediates a range of immunological responses as a multitude of insults from the outside world attempt to breach the barrier. Sometimes called the largest of the human organs, these are just a few of the important functions skin accomplishes regularly.
To conduct these functions our epidermis is stratified, each layer with its own unique function. The major layers are as follows, from the outer-most stratum to the inner-most:
- Stratum corneum. This layer is in direct contact with the outside world and consists of a variable number of layers of dead, flattened, scale-like squamous cells, which continually slough off. Although the cells in this layer are without nuclei and are not "living," they aid the body in their ability to hydrate and simultaneously prevent water loss, and through connective proteins provide a supple sheathing for the underlying layers.
- Stratum lucidum. This layer likewise consists of dead, flattened cells that migrate up through lower layers. Melanocytes in this layer—which were pigment-producing while in lower layers (i.e., stratum basale)—now react to light, as the descriptor lucidum implies, determining the darkness of skin.
- Stratum granulosum. This layer is of particular interest as it is where filaggrin proteins reside, or, in the case of people who are carriers of the FLG mutations, contains dysfunctional filaggrin, or is missing filaggrin entirely. Filaggrin is integral to a fully functional epidermal barrier. Dysfunctional or missing filaggrin compromises the barrier and gives rise to atopic disease in a large proportion of carriers. Filaggrin's role in this layer will be discussed more fully below.
- Stratum spinosum. Keratinization of basal cells, also called keratinocytes, the epidermal "stem" cells produced in the next-lower stratum basale, occurs in the stratum spinosum. Bipolar lipids—fatty molecules that possess a water-loving (hydrophilic) end and a water-repelling (hydrophobic) end—are also produced in this layer, conferring watertight properties to skin. Keratinocytes are critical components in the immune response system, modulating inflammation by secretion of inhibitory or stimulating cytokines as conditions warrant.
- Stratum basale. Epidermal "stem" cells are formed in this lowest stratum of the epidermis. These are undifferentiated cells continually undergoing mitosis, differentiating into specific epidermal cell types and migrating into the upper layers.
Barrier Function, Eczema, Allergies, and Infection
The mutations that cause loss of function or missing filaggrin have been shown to be a major predisposing factor to the development of atopic eczema, eczema-related asthma, and allergic rhinitis. As many as 10% of European populations carry these gene deficiencies.
It has been generally thought that abnormalities in a patient's immune response were primary in the pathogenesis of atopic eczema. Dysregulation of pro-inflammatory T-helper cells 1 and 2 (TH1, TH2), mast cell hyperactivity, increased IgE production, and dysfunctional dendritic cell-signaling all characterize the immune response in the course of the disease. Current treatments have targeted TH2-mediated inflammation to relieve symptoms with some success.
Additionally, the loss of key antimicrobial peptides in the skin that fight infection, as well as the impairment of pattern-recognition receptors in the skin that identify attacking microbes and signal for an immune response, combined with a compromised barrier, also play a role in disease progression.
In this view, the pathogenesis of atopic disease is a compromised epidermal barrier, in concert with these other problems, triggering the immune response, inflammation and pruritus, the underlying, largely unknown conditions causing itch, which in turn further disrupts the skin.
With an impaired microbial recognition and response system, opportunistic infections, often from staphylococcal bacteria and some cutaneous viruses, are more common in eczema sufferers, contributing to the discomfort and complications of the disease.
Furthermore, it has been hypothesized that a certain percentage of individuals with filaggrin deficiency go on to develop eczema-related asthma when allergens to which their immune systems have been exposed through the compromised epidermis enter the lungs and initiate an immune response.
Null mutations in filaggrin, leading to non-functioning or missing filaggrin, appear to associate with early-onset atopic dermatitis that persists into adulthood, and more severe eczema-related asthma.
An Evolutionary Role?
Through study of another disease, ichthyosis vulgaris, a similar keratinizing disorder, two particular mutations were discovered that result in the complete absence of filaggrin expression, and that about 10% of European populations carry these gene alterations. Further work showed that these mutations were also prevalent in atopic disease sufferers.
The fact that these two mutations exist in 10% of the population of European descent, and arose as separate mutations accomplishing the same defect may indicate a "heterozygote advantage" that conferred through natural selection a preference for a particular trait to be expressed in the offspring of the carriers. Two independent mutations leading to the same loss of function of a gene are not easily explained by random genetic drift.
Human beings are diploid organisms—having two copies of each gene encoded in their DNA. Carrying this mutation on one of the copies of the FLA gene, a heterozygous mutation, may have conferred an evolutionary advantage to the carriers by giving them, through their minor barrier defect, a method of "natural vaccination" and increased immunity to tuberculosis, influenza, or plague. Repeated, low-level exposure to the pathogens of these diseases may have allowed the carriers to survive outbreaks of these diseases and pass along the mutations. The authors of work relating to filaggrin and atopic disease ask the question, "Is atopic disease a modern plague suffered by descendents of the survivors of ancient plagues?"
Filaggrin Plays a Role and is Not the Whole Story
It is estimated that 50% or more of children with moderate to severe atopic dermatitis carry mutations in the FLA gene. But because these genetic mutations are likely ancient, they are not able to explain the observed increase in atopic disease over the past decades. It is likely that the barrier defects that result from dysfunctional or missing filaggrin are aggravated by environmental conditions and substances in common use that may lower the threshold for onset of the disease. Dry environments, including those created by certain heating systems, and increased exposure to detergents and soaps may exacerbate the barrier defect. How one's environment or exposure to substances may trigger the immunological response typical of the disease is not clear.
One hypothesis has been asserted and disputed, in turn, but still warrants consideration as a contributing mechanism. The "hygiene hypothesis" postulates that lifestyle changes in more recent decades leading to overall greater cleanliness of living conditions and reduced exposures to viruses and bacteria in the first year of life may contribute to increases in atopic eczema and eczema-related asthma.
Endotoxin is a lipopolysaccharide found in the outer membrane of certain bacteria. An inverse relationship appears to exist between children exposed to higher concentrations of endotoxins in their first year of life and the incidence of eczema at age 1 year. Those children in inner-city and non-farm households that were exposed to higher levels of endotoxins in their environment were less likely to have eczema at 1 year. It has been postulated that higher ambient endotoxin exposure suppresses the immune response that involves T-helper 2 cells and the formation of IgE, an immunoglobulin involved in powerful allergic immune reactions. Early childhood exposure to endotoxins may play an important role conferring tolerance later in life.
Antioxidants and Diet
Changes in diet over the past two decades have led researchers to think that diets that lack in green vegetables, fruits and potatoes, as well as sharp changes in the intake ratio of omega-6 to omega-3 fatty acids is associated with increases in atopic conditions such as eczema, eczema-related asthma, and allergies. Higher intake of linoleic and arachidonic acids (both n6 polyunsaturated fatty acids) through increased use of margarine, corn and certain other vegetable oils as opposed to butter, lard, nuts and seeds, together with decreased intake of oily fish, rich sources of eicosapentaenoic and docosahexaenoic acids (both n3 polyunsaturated acids), represent changes in the Western diet that have resulted in a higher prevalence of atopic conditions.
Epidemiological studies have reported benefits from dietary antioxidants in adults and children in relation to eczema and related atopic diseases. Antioxidant intake, specifically vitamins E and C, during pregnancy has likewise been associated with better outcomes for children regarding eczema in early childhood. And, women may lend protection to their children from eczema and allergic diseases by the consumption of apples and fish (consume the smallest wild-caught fish to reduce intake of heavy metal; alternatively women can consume a molecularly distilled fish oil supplement) during their pregnancies. A recent European study showed benefits for eczema risk in young children associated with the intake of dietary nutrients vitamin E, folic acid, and iron.
It is not clear how the diets of adults, children or pregnant women might positively influence a barrier defect that is the result of mutations in the FLG gene, but there is no question that sound nutrition is the substrate from which all healthy tissues are regenerated.
What We've Learned—Genes and Environment Interact
A genetic basis has been established for the occurrence of eczema. Mutations in the FLA gene can lead to loss of function of the epidermal protein filaggrin, or its complete absence. Filaggrin is an integral component in the formation of the epidermal barrier, and its loss of function, or absence can lead to dysfunction of the epidermal barrier. It has been estimated that half or more of children with severe to moderate eczema are carriers of the mutations that inhibit filaggrin function. A prenatal diet rich in antioxidants, fruits and vegetables, and a proper ratio of omega-3 to omega-6 fatty acids has been associated with a decreased risk of eczema and eczema-related atopic conditions in early childhood. Further opportunity remains throughout life to provide one's systems with a ready supply of nutrients as the substrate for daily healthy tissue regeneration.
Putting It Together and Finding Your Eczema Solution
While a cure is still a goal yet to be realized, there are many natural options that can help the juvenile or adult eczema sufferer take part in managing—often reducing—the severity of the condition. A combination approach that includes identifying a healthy meal plan and avoiding dietary triggers, together with the use of natural herbs and other nutritional supplements, topical gels or ointments, and stress-reducing techniques are all ways to naturally reduce discomforting symptoms of eczema.
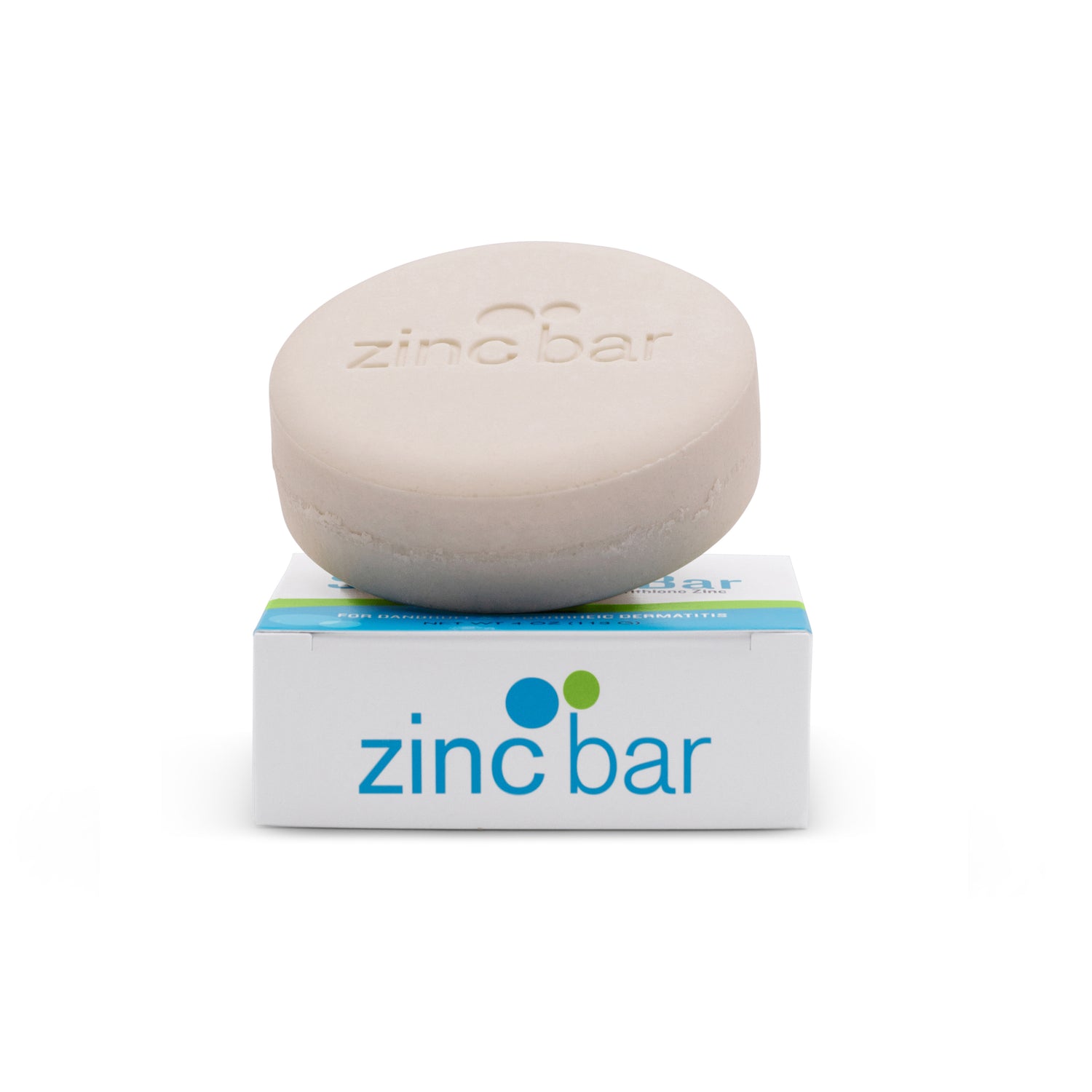
You should try cleansing your problem skin with a combination of zinc pyrithione and sulfur/salicylic acid (two different products - alternating use) to see if it helps.