Nummular Dermatitis
Overview
Nummular dermatitis is an inflammatory skin irritation characterized by its round, coin-shaped lesions. Sometimes referred to as discoid eczema, it affects approximately 2 in every 1000 people in the United States and is most prevalent in middle-aged patients. Men are more commonly affected by this skin condition, with their first outbreak generally occurring between the ages of 55 and 65. Women affected by this form of dermatitis typically experience their first outbreak much earlier in life, between the ages of 15 and 25. It is extremely rare to see this type of dermatitis in children.
Symptoms and causes of nummular dermatitis
The word nummular derives from the Latin word for coin, and nummular dermatitis is most well known for the unique coin-shaped lesions that appear on the skin at the onset of an outbreak. These classic discoid lesions usually appear on the legs, but can also be found on the hands, feet, torso and arms. They often start off as small red itchy and burning blisters that eventually range in size from one to four inches in diameter. As the rash continues its life cycle, the blisters may fill and weep fluid. As the rash nears the end stages, the skin on these raised patches can become crusty, scaly, and raw. If the crusty layer of the rash has a yellowish color it may signal infection.
The patches may begin to heal from the center of the coin shape outwards toward the edges, creating a ring-like appearance. The skin in-between the circular patches will be clear but may be dry and sensitive. Once cleared the lesions may leave the healed skin looking darker or lighter than the surrounding skin. This discoloration usually resolves, but if the rash has occurred beneath the knee the changes in pigmentation may be permanent.
The exact cause of nummular dermatitis remains unknown, though certain risk factors and triggers of the disease have been identified. It is not uncommon for a patient's personal or family history to show allergies, asthma, atopic dermatitis, or similar diseases. There are also a number of conditions that can trigger or worsen the condition:
- Weather conditions—extremely hot, cold, humid, or dry conditions are irritating
- Wool, or any tight fitting clothing that is not cotton
- Frequent bathing—more than once per day
- Stress
- Harsh detergents, soaps, or solvents
- Injury to the skin, such as a burn, insect bite, or abrasion
- Bacterial skin infection
- Isotretinoin—a commonly prescribed medication for acne
In addition, some researchers believe that those suffering with nummular dermatitis show a heightened sensitivity and even an allergy to some materials. These include but are not limited to:
- Rubber
- Nickel
- Neomycin and other topical antibiotics
- Formaldehyde
- Mercury—believed to be rare, but some patients recover only when all their mercury fillings are removed, leading to the belief that the reaction was due to inhaling mercury vapor
Diagnosis and medical treatment of nummular dermatitis
Due to the unique appearance of nummular dermatitis, a visual diagnosis can be made in most cases. If there is any doubt a physician may do a skin biopsy to rule out any other conditions.
There is no cure for nummular dermatitis, and in most cases the condition is chronic and persistent. The rash will typically go through phases of remission and flare-ups. Some patients clear the rash within a year, whereas others have recurring outbreaks for many years. The rash does tend to recur at the original site of infection.
Treatment of nummular dermatitis is centered around preventing future flare-ups, and when a flare-up does occur by treating the symptoms of the rash. Preventing flare-ups can be done through proper skin care and avoiding irritating conditions and substances. Here are some measures you can use to treat and prevent repeat flare-ups.
- Protect the skin from injury.
- Moisturize—apply lotion to the skin after bathing and a couple of times daily.
- Take cool to lukewarm showers (hot showers dry out the skin).
- Avoid activities that cause excessive sweating and overheating.
- Avoid extremely hot and cold weather conditions.
- Use a humidifier in cold dry conditions.
- Avoid fabric softener and dryer sheets.
- Use mild soaps and detergents that are fragrance-free and dye-free.
- Wear loose-fitting cotton clothing.
- Avoid contact with harsh chemicals such as petroleum products, fertilizers, or gasoline.
If a mild outbreak does occur it can often be contained and treated with non-prescription topical cortisone creams or gentle hypoallergenic lubricating creams to relieve the itching and burning. If the outbreak is more aggressive, your doctor may recommend prescription-strength topical cortisone creams or steroidal creams, oral antihistamines, cortisone or steroids, or injectable cortisones or steroids. For outbreaks that are potentially infected or that fail to respond to treatment, a course of oral antibiotics, topical coal tar products, and ultraviolet light therapy may be used.
Patients with nummular dermatitis are at distinctly increased risk of developing secondary allergic contact dermatitis which, though not believed to be causal, may certainly contribute to the severity and chronic nature of their dermatitis. By identifying triggers, patch testing has the potential to improve the quality of life in these patients. In the case of suspected allergies, a patch test may be done.
There are two methods of patch testing, the most frequently used being the Finn chamber method. A multiwell aluminum patch is filled with the suspected substances and taped to the skin, usually on the patient's upper back. The patch is left on the patient's skin for a 48-hour period, then removed and an initial reading of the skin taken. A second reading of the skin is done a few days later. The second method of testing is to apply the suspected substance directly to the skin with a dressing applied over it. Again, after 48 hours an initial skin reading is taken and a few days later a second reading taken. Repeated testing may be necessary to identify the offending substance with certainty.
Herbal treatments for nummular dermatitis
Several all-natural herbal methods can be used to help relieve the pain and itching associated with a nummular dermatitis outbreak. Certain herbs have antiseptic and anti-inflammatory properties that can help to relieve the symptoms. These skin-healing herbs include the following:
- Calendula (flower heads), licorice root, and ginkgo all have antiseptic and anti-inflammatory properties. They can be applied topically in the form of lotions, oils or ointments to reduce itching and inflammation.
- Aloe vera gel and the juice and leaves of the common plantain (Plantago officinalis) can be applied topically to the affected areas to help soothe skin irritations associated with dermatitis.
Some find the following herbal pastes helpful in relieving the intense itching associated with nummular dermatitis:
- Green clay and goldenseal root in equal parts
- Equal parts salt, water, clay, and peppermint oil
- Calamine lotion
- Coal tar lotions, shampoos, and bath oils
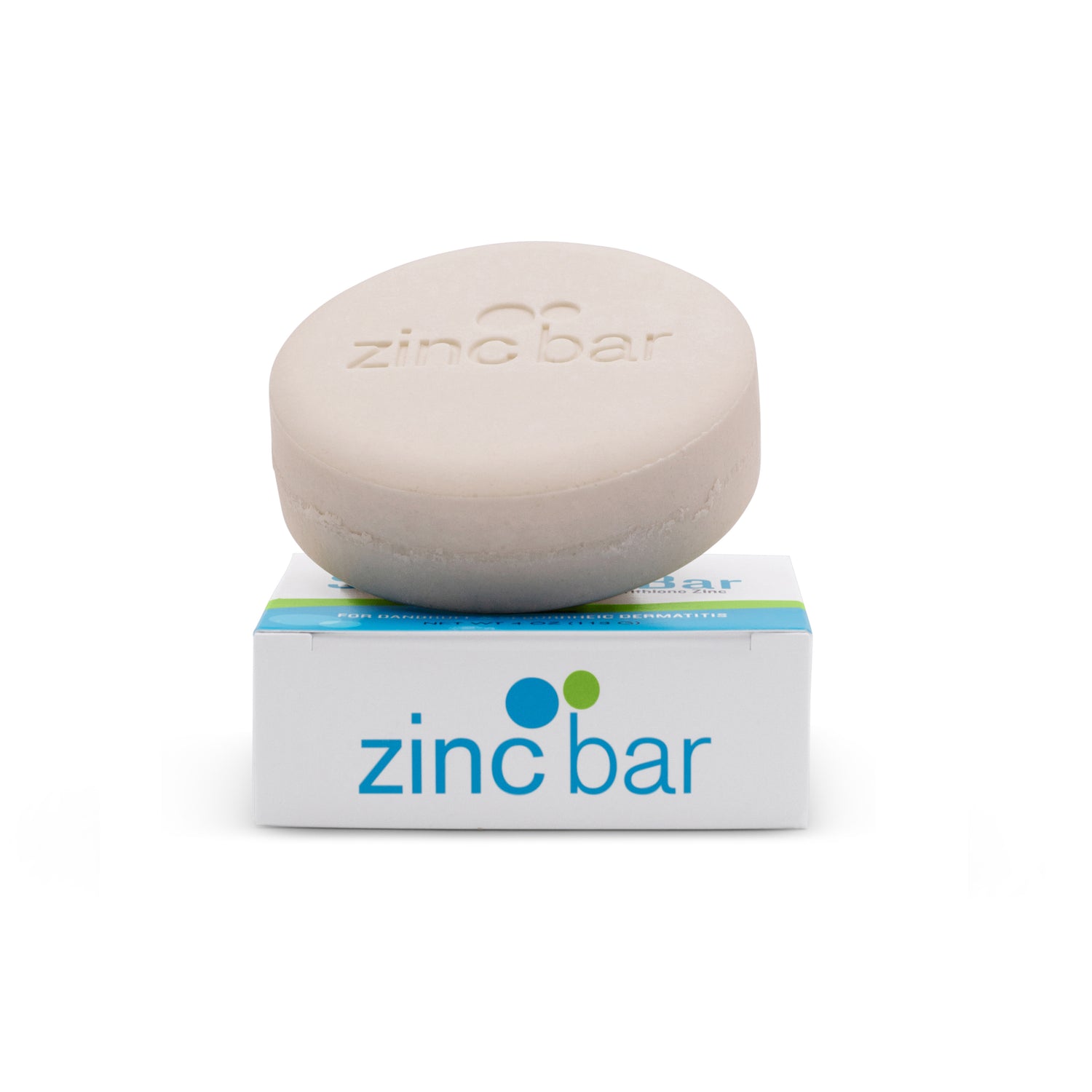
Pyrithione zinc treatment
Pyrithione zinc has long been recognized for its unique skin-healing properties. Included in those healing properties are its ability to alleviate the itching and burning symptoms associated with nummular dermatitis.
Pyrithione zinc is an antiseborrheic, which means that it helps to prevent or relieve excessive secretions of oil by the sebaceous glands. These glands lie beneath the skin and work to soften and lubricate the skin and hair. If they become overactive, however, as happens during an outbreak of dermatitis, the skin can become inflamed and irritated. By its ability to modulate the function of the sebaceous glands, pyrithione zinc can limit these outbreaks and reduce flare-ups of atopic dermatitis.
Pyrithione zinc also has antifungal and antibacterial properties, which may help reduce skin inflammation associated with secondary infection in patients with dermatitis. Topical zinc pyrithione is generally recognized as a safe and effective treatment for reduction in the symptoms associated with dermatitis.