Stasis Dermatitis
Overview
Stasis dermatitis is an inflammatory skin condition that develops secondary to fluid build-up, or blood pooling (stasis), just under the skin as a result of problematic circulation. While it can occur in people as early as their teen years, it rarely develops in adults under the age of 40, where advancing age is the primary risk factor for circulatory decline. In the United States it affects about 15-20 million individuals over the age of 50, with incidence among women slightly higher than among men.
Note: If leg swelling or stasis dermatitis develops, contact your healthcare provider for an appointment or referral to a dermatologist. It is particularly important to seek immediate medical attention in the case of rapid onset of stasis dermatitis, as this can be indicative of deep venous thrombosis (DVT), a particularly dangerous type of blood clot.
Symptoms and causes of stasis dermatitis
A case of stasis dermatitis can develop literally overnight, or slowly and over such a long period of time that the swelling may go unnoticed for some time. If marked swelling occurs suddenly, you should always seek medical treatment immediately, as this can be indicative of deep venous thrombosis (DVT). The build-up of fluid underneath the skin typically begins just above the ankles, and may work its way up to just below the knee in a "gaiter" distribution.
The predisposing factor in stasis dermatitis is insufficient venous return. This venous insufficiency can be due to varicosities in the legs (hence the alternate name, varicose eczema), which in turn can lead to increased pressure on capillaries in the extremities. This results in leaking of blood fluid and cells from the capillaries, where it collects in the intracellular spaces rather than being drawn back into the circulatory system appropriately and in a timely fashion.
This fluid accumulation can make it difficult for the circulatory and lymphatic system to adequately feed your tissue cells and subsequently dispose of cellular waste. The result is that the tissue becomes malnourished and fragile, making it vulnerable to increased sensitivities, allergies, and tissue damage.
The rash associated with stasis dermatitis can have the following characteristics:
- Thin, inflamed, tissue-like skin
- Itching, which can be severe
- Itching, which can be severe
- Tingling
- Red skin spots, caused by small deposits of hemosiderin from the breakdown of red blood cells
- Dry and scaly patches of skin
- Darkening of the skin, which appears reddish brown (hyperpigmentation)
- Thickening of the skin, caused by ongoing scratching
- Slow-to-heal, painful, open sores (venous ulcers)
- Discolored pus may ooze from infected skin
The swelling that prompts and accompanies stasis dermatitis can be exacerbated by a number of factors. The leading associated risk factor for swelling is advanced aging. Other risk factors include:
- Obesity
- Blood clot (deep venous thrombosis)
- Heart condition, including congestive heart failure (CHF)
- Kidney failure
- Sedentary lifestyle
- Varicose veins (varicosities)
- High blood pressure (hypertension)
Those who have any of the above conditions and develop stasis dermatitis are also at a higher risk for developing contact sensitivity or dermatitis. Most notably, allergic contact dermatitis is a problem in those affected, and patch testing may help to elucidate any sensitivities prior to instituting topical agents to help heal ulcerations.
Stasis dermatitis patients are also at increased risk for cellulitis, where a bacterial pathogen gains entry at a crack or small tear in the skin's surface, initiating infection which then migrates into the subdermal layers and spreads to adjoining tissues, causing a venous stasis ulcer.
Diagnosis and medical treatment of stasis dermatitis
A diagnosis of stasis dermatitis is made based on the patient's medical history, investigating any conditions that may cause the swelling, as well as observation of the skin rash. Testing for other skin conditions as well as circulation patterns of the body may include:
- Blood tests
- Blood flow to the legs is evaluated by Doppler testing
- Patch testing to determine contact allergies and/or other skin sensitivities
- Biopsy of infected skin
Stasis dermatitis is often a long-term condition that remains present as long as the swelling persists. Immediate treatment is focused on decreasing and even eliminating the fluid build-up in the legs. This can be achieved through a combination of a lifestyle changes and prescription medications.
- To improve circulation when sleeping, resting or sitting, elevate the legs above the heart.
- When awake, use compression stockings (e.g., TED) to improve circulation.
- While up and about, use compression in combination with a hydrocolloid dressing or Unna boot to facilitate healing of venous ulcers.
- Treat congestive heart failure and high blood pressure with a low-dose diuretic.
- Strict bed rest may be necessary at initiation of treatment or onset of infection.
Once the swelling has subsided and the rash has cleared up, treatment is more focused on prevention of future swelling. Some steps which are used to rid the body of the initial swelling will be necessary to continue for prevention: compression stockings; regularly elevating the legs; and treating congestive heart failure. In addition to those steps, it is recommended that you take regular walks, avoid standing or sitting still for long periods of time and last but not least, moisturize the skin on the legs at least once daily. All of the above measures can likewise help to prevent an existing case of stasis dermatitis from worsening.
Treating the rash itself is centered on relieving the pain, tingling, and itching, and preventing any open sores and secondary infection from developing. If the outbreak has not progressed too far, a soothing compress of gauze pads and water or aluminum acetate can be used. This not only helps ease the itching but helps keep the skin clean, which protects against infection.
If the condition develops with increased redness and ulcers, then a low- to medium-dose topical steroid with zinc oxide may be prescribed to aid in the healing process. However, it should be noted that topical steroid creams should not be applied directly onto an open ulcer, as they can inhibit healing. Oral and topical antibiotics may be additionally prescribed if the skin has become infected or a case of cellulitis has developed.
Stasis dermatitis does cause the skin to become very easily irritated, so proper wound care and cleanliness are key components to healing. In addition, any products containing ingredients associated with the development of contact dermatitis should be avoided, including antibiotic creams; first-aid creams; lotions containing alcohol, witch hazel, or lanolin. These chemicals can exacerbate a localized, and in worse cases a systemic, inflammatory response.
Herbal treatments
In some cases, all-natural herbal methods can be used to help soothe the pain and itching associated with milder forms of stasis dermatitis. For best results, however, they should always be used under the guidance of a qualified herbalist or licensed naturopathic healthcare provider.
These herbs have antiseptic and anti-inflammatory properties, which may help to relieve the symptoms:
- Calendula (flower heads), licorice root, and ginkgo all have antiseptic and anti-inflammatory properties. They can be used topically, in lotions, oils or ointment form, on the affected area to reduce itching and inflammation.
- Aloe vera gel and the juice from common plantain leaves (Plantago major) can be applied topically to the affected areas to help soothe skin irritations associated with dermatitis.
Herbal pastes can also be prepared to help relieve the itching associated with dermatitis:
- Green clay and goldenseal root in equal parts
- Equal parts salt, water, clay, and peppermint oil
- Calamine lotion
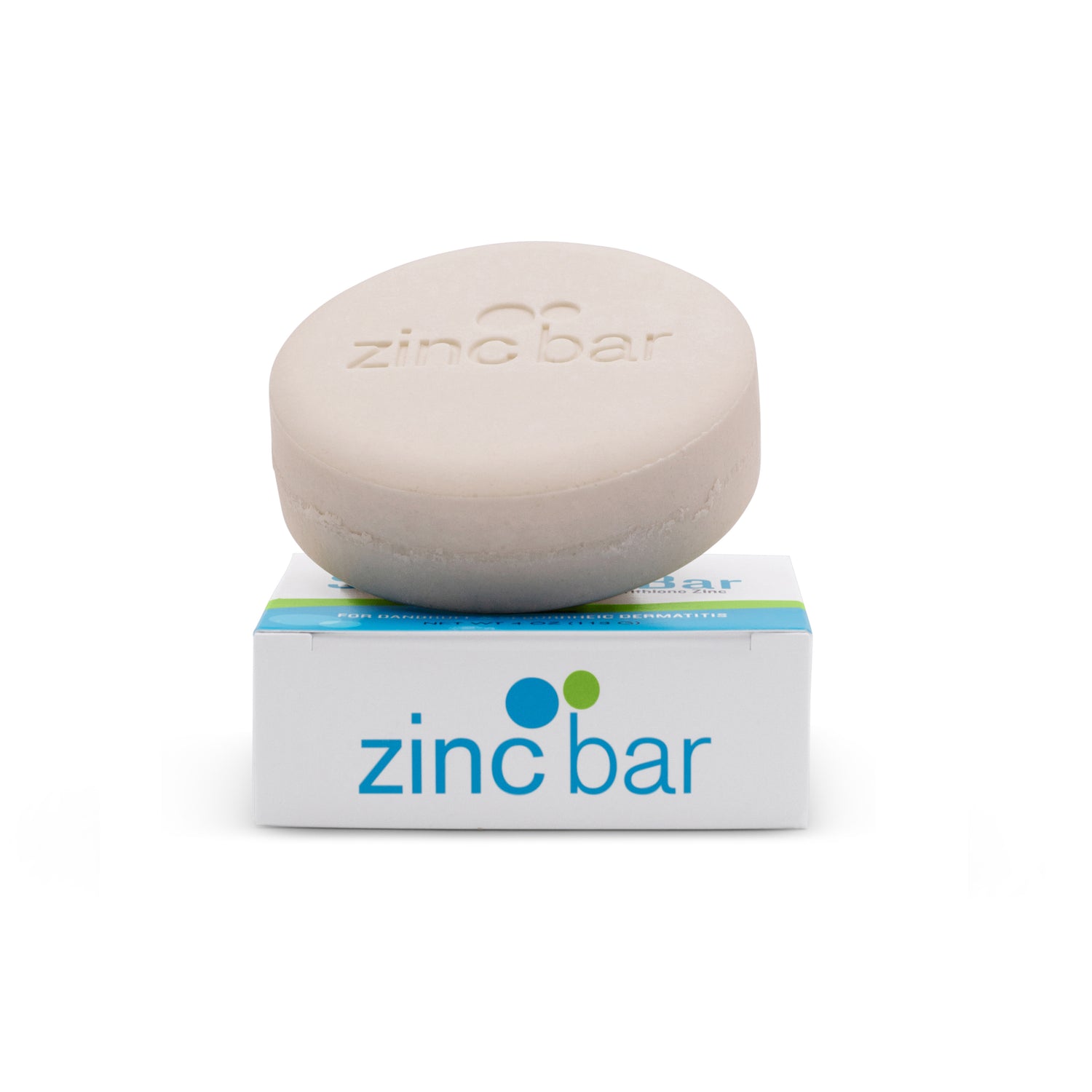
Zinc treatment
Pyrithione zinc has been recognized for centuries for its unique healing properties. Included in those healing properties are alleviation of itching and burning associated with dermatitis symptoms. Pyrithione zinc also has antifungal and antibacterial properties, which may help reduce skin inflammation associated with dermatitis. Topical zinc pyrithione is generally recognized as a safe and effective treatment for reduction in the symptoms associated with certain forms of dermatitis.
In the case of stasis dermatitis, zinc is often used in connection with an Unna's paste boot, a moist, zinc-impregnated paste bandage that provides both compression and topical treatment. The classic Unna boot entails a stretched wrap filled with calamine, zinc oxide, glycerine, sorbitol, gelatin and magnesium aluminum silicate, to be applied to the affected area. Once applied, the boot will harden to a level that is slightly less than that of a cast. The compressive, supportive nature of the boot helps to reduce the swelling, and the gelatin/zinc mixture protects the skin from irritation and hastens the healing process. In the beginning the boot needs to be changed every two to three days; however after the initial healing it can be left on for a week at a time.
One drawback of the Unna boot is that it does not accommodate changes in leg swelling particularly well. Many comparative studies of different management techniques, including compression with Unna boot, traditional paraffin gauze dressings, and other occlusive dressings, have been made. In some cases, studies report better patient comfort and compliance when treated with a combination of compression and a moist, occlusive dressing, such as a hydrocolloid dressing, to heal venous stasis ulceration.
In summary, the condition of stasis dermatitis can be quite serious and chronic, with numerous complicating factors and sequelae. However, with careful evaluation, follow-up, and a maintenance program tailored to an individual's needs, along with education and counseling to improve understanding of the condition, most stasis dermatitis patients can be kept comfortable and free of ulceration.